India ranks uterine cancers, particularly endometrial cancers, as the fourth most common gynaecological cancer. Globally, however, endometrial cancer ranks as the second most prevalent and the fourth leading cause of cancer-related deaths among women as of 2020.1 Between 1990 and 2021, the number of cases has steadily risen, particularly among women of reproductive age. Despite this increase in diagnoses, improvements in treatment and care have helped reduce the overall disease burden.
Synopsis
- The Fundamentals of Uterine Cancer – Common Types and Symptoms
- What are the uterine cancer symptoms?
- Common Uterine Cancer Causes and How to Reduce Your Risk
- Factors That Help Reduce Uterine Cancer Risks
- Uterine Cancer – Methods of Diagnosis and Treatment Options
- Stages of Uterine Cancer – How is it Determined?
- What are uterine cancer treatments?
- What are the post-treatment follow-ups for uterine cancer?
- Palliative Treatment for Uterine Cancer – Is It the End of Life?
- Conclusion
The Fundamentals of Uterine Cancer – Common Types and Symptoms
The uterus, also known as the womb, is a hollow, pear-shaped organ located in a woman’s pelvis where the baby grows during pregnancy. It plays a vital role in menstruation, fertility and gestation.
Uterine cancer arises when abnormal cells in the uterus begin to grow uncontrollably. It is mainly classified into two types: endometrial cancer and uterine sarcoma. Endometrial cancer, the more common and treatable form, starts in the inner lining of the uterus. In contrast, uterine sarcoma originates in the muscular wall of the uterus (myometrium) and is a rare, more aggressive, and challenging condition to treat.
80% of endometrial cancers are adenocarcinomas (i.e., cancer that develops from glands that line the organs), primarily endometrioid carcinomas. Rare types include serous adenocarcinoma, adenosquamous carcinoma, uterine carcinosarcoma, primary pure squamous cell carcinoma of the endometrium, and uterine clear cell carcinoma, each varying in aggressiveness and spread. On the other hand, uterine sarcomas are classified based on where the cancers begin. These include uterine leiomyosarcoma, endometrial stromal sarcomas, and undifferentiated sarcoma.
What are the uterine cancer symptoms?
There are several uterine cancer symptoms, with the most common one being unusual bleeding, especially in post-menopausal females. Other signs of uterine cancer include:
-
Heavy vaginal bleeding in between periods before menopause
-
Continuous periods without a break
-
Lower abdominal pain or cramping
-
Vaginal discharge with unpleasant smell, especially post-menopause
-
Change in bowel habits
-
Difficulty urinating
-
Unexplained weight loss
Note that the signs of uterine cancer may resemble those exhibited by other conditions affecting reproductive organs. Therefore, it is important to consult your doctor and rule out the condition.
Common Uterine Cancer Causes and How to Reduce Your Risk
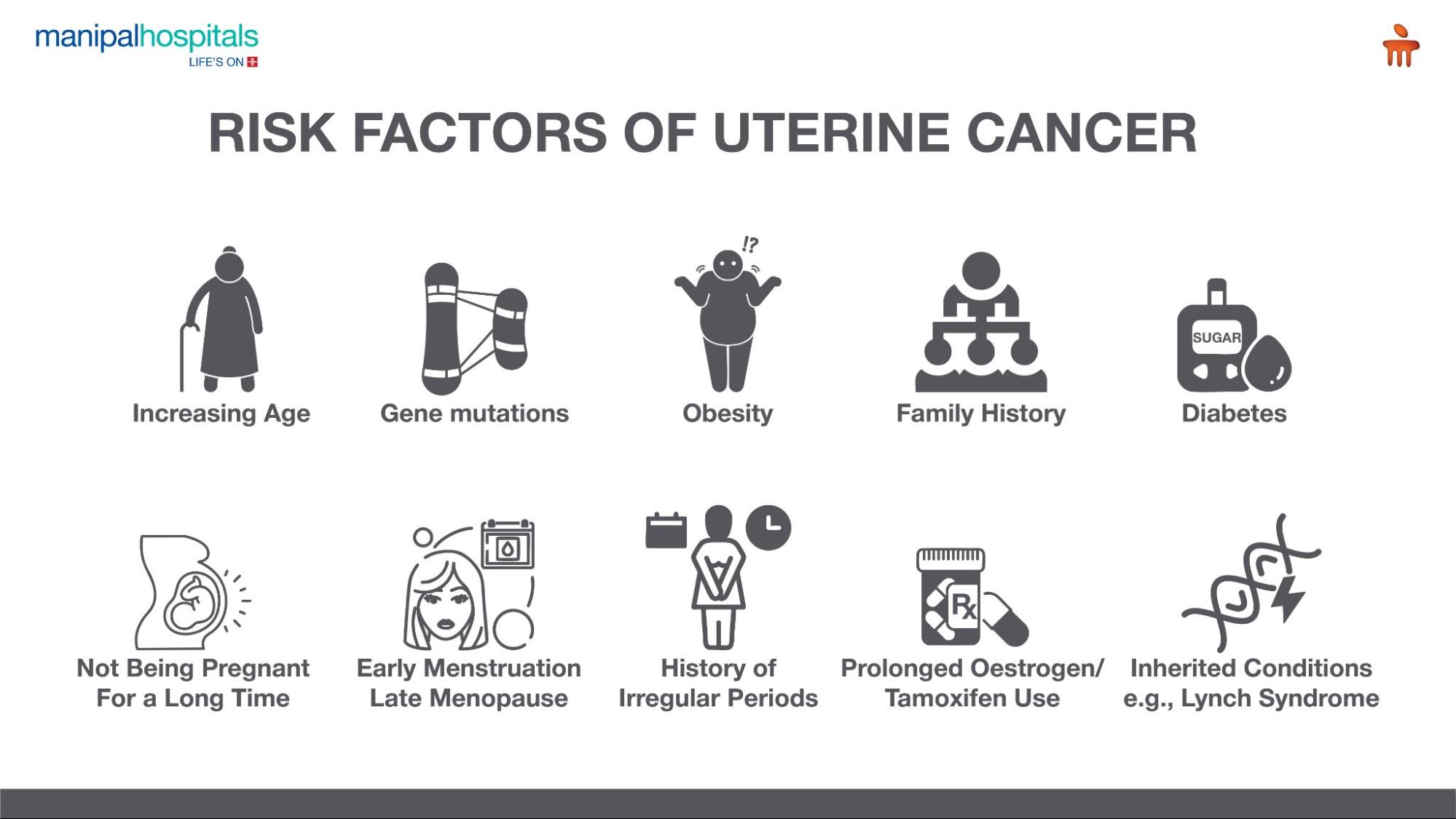
The exact cause of uterine cancer remains unclear, but it’s largely linked to genetic mutations that trigger abnormal cell growth. Other risk factors include:
- Oestrogen Exposure: Long-term, unopposed exposure—such as from oestrogen-only hormone therapy, early menstruation, or late menopause—raises risk. Women who’ve never been pregnant also face higher exposure.
- Endometrial Hyperplasia: Although it is non-cancerous, this abnormal thickening of the uterine lining has the potential to develop into cancer.
- Age: Risk increases with age, especially for those who have crossed 50 and have achieved menopause.
- Hormone Therapy for Breast Cancer: Tamoxifen, especially when used for over 2 years in postmenopausal women, elevates risk.
- Obesity & Comorbidities: Obesity, diabetes, hypertension, and PCOS contribute to a higher risk due to hormonal imbalances - Corpus Cancer Syndrome. Experts point out that six out of 10 cases of uterine cancer are attributed to being overweight or obese.
- Genetics: Conditions like Cowden syndrome or a family history of uterine colorectal cancer significantly increase susceptibility. For example, hereditary nonpolyposis colorectal cancer (HNPCC) or Lynch syndrome, a genetic condition, can increase the risk of uterine cancers, as well as colon cancer.
Factors That Help Reduce Uterine Cancer Risks
Some of the factors that can help in reducing uterine cancer risks include:
-
Taking hormone therapy medicines containing oestrogen along with progestin post menopause.
-
Maintaining a healthy weight and exercising
-
Using a birth control pill containing progestin and oestrogen
-
Intrauterine contraceptive devices (IUDs) – either progesterone- or copper-containing – are known to decrease the risk of endometrial cancer
-
High progesterone levels during pregnancy offer protection against endometrial cancer, with multiple pregnancies and breastfeeding further reducing a mother’s risk.
-
Undergoing annual health checkups, especially in high-risk populations.
Uterine Cancer – Methods of Diagnosis and Treatment Options
Gynaec oncologists often use a multidisciplinary approach to diagnose and treat uterine cancer, with support from other experts in Medical Oncology, Pathology, Radiology, Genetics and Palliative Care. The process of diagnosing uterine cancer usually begins with a thorough review of your symptoms and medical and family history, along with lifestyle considerations. In some cases, a Pap smear may be suggested as an initial screening test. If signs point to uterine cancer, additional diagnostic tests are carried out to confirm the diagnosis.
-
Transvaginal ultrasound (TVUS): Uses a vaginal probe to create images of the uterus and pelvic area via sound waves. The TVUS can screen for Lynch syndrome, help pinpoint abnormal uterine bleeding, and monitor patients with endometrial hyperplasia.
-
Endometrial biopsy: Involves removing a small tissue sample from the uterine lining to examine for the presence of cancer cells. The primary purpose of an endometrial biopsy is to detect abnormal bleeding, particularly after menopause or in between periods. It also helps to screen for the presence of precancerous cells, i.e., endometrial hyperplasia
-
Dilation and Curettage (D&C): It involves scraping tissue from the uterine lining with a curette, which is then analysed in a lab. D&C is often employed if the biopsy does not provide enough tissue for diagnosis or if the results are inconsistent.
-
Hysteroscopy: Allows visual inspection of the uterus using a lighted tube with a camera. Any suspicious areas seen can be biopsied. If imaging shows suspicious findings, hysteroscopy may be used as part of the initial assessment before D&C. The procedure also allows for targeted tissue sampling for biopsy.
Stages of Uterine Cancer – How is it Determined?
If cancer is confirmed, staging helps determine its spread and severity using the FIGO system (Stages I–IV), where lower stages indicate less advancement. This staging, along with imaging and pathology results, helps guide the treatment plan.
|
Stage |
Description |
|
Stage I |
The cancer is confined to the uterus |
|
Stage II |
The cancer has reached and spread to the cervix |
|
Stage III |
The cancer has spread to nearby areas like vagina, ovaries and lymph nodes |
|
Stage IV |
The cancer has spread to distant organs, such as the urinary bladder, rectum, lungs, bones, etc. |
Prognosis (i.e., expected disease outcomes or course) is highly favourable for Stage 1, with 90% of patients diagnosed at the early stage having a 5-year survival rate. The prognosis of stage II is relatively good, with 75% of patients surviving five years or more. In stage III, the prognosis becomes more guarded, with the survival rate dropping to around 50%. The prognosis for patients in stage IV is poor, and palliative care, or improving quality of life, is the main focus of treatment.
What are uterine cancer treatments?
There are various uterine cancer treatments, and each is recommended based on the patient’s condition. In select early cases, fertility-sparing treatment may be considered for younger women.
-
Surgery: Often the first step. Based on the patient’s condition and nature of the tumour, the procedure may also include removal of the uterus, cervix, ovaries, fallopian tubes, draining lymph nodes, and omentum. Minimally invasive surgery is the preferred surgical approach. Side effects can often include infertility, menopause, potential bladder and bowel movements and sexual problems.
-
Radiation Therapy: Uses high-energy beams to destroy cancer cells. It can be given externally (External Beam Radiation) or internally (Brachytherapy). Common side effects include fatigue, redness in the skin, bladder irritation, bowel changes, vaginal dryness or discharge, or more.
-
Chemotherapy: Uses medications, given orally or intravenously, that circulate through the bloodstream to destroy cancer cells or reduce tumour size. It can be administered before surgery to shrink tumours or after surgery to prevent recurrences. Side effects usually include nausea, vomiting, hair loss, and changes in appetite. In rare cases, organ damage and infection can occur.
-
Hormone Therapy: Typically used in advanced stages, this treatment reduces hormone levels or blocks their action to slow the growth of hormone-dependent cancer cells. Common side effects include fatigue, hot flashes, weight gain and mood swings. In serious cases, it could lead to bone loss, blood clots and an increased risk of other cancers.
-
Targeted Therapy: Attacks specific proteins or genes in cancer cells, limiting their ability to grow or spread. Side effects usually include nausea, fatigue, skin problems, diarrhoea, or specific side effects, like heart problems, blood clots, or lung damage.
What are the post-treatment follow-ups for uterine cancer?
After uterine cancer treatment, follow-up visits are done every 3–4 months for the first 2–3 years, then every 6 months and annually thereafter. These visits include physical and pelvic exams, checking lymph nodes, and tests like chest X-rays, CT scans, or tumour markers (e.g., CA 125) to detect recurrence. If cancer returns, further treatment options are explored.
Palliative Treatment for Uterine Cancer – Is It the End of Life?
Palliative treatment is usually recommended when the cancer is at an advanced stage. While often misunderstood as end-of-life care, it can benefit patients with advanced uterine cancer at any stage. The goal is to enhance patients’ quality of life by managing pain and symptoms, reducing side effects and slowing the progression of the disease.
Palliative therapies usually involve radiation, chemotherapy or hormones to relieve pain and manage symptoms. It also supports emotional, social, and spiritual needs, offering guidance for patients and their families.
Conclusion
Research and improvements are being carried out globally, even though uterine cancers are increasing worldwide. Doctors are focusing more on precision medicine to improve patient care and outcomes. Detailed testing of tumour genes, combined with new targeted treatments, provides hope for both doctors and patients. Promising developments include Immunotherapy, Newer Hormonal Therapies, Antibody-Drug Conjugates and Targeted Therapies.
If you or your loved ones experience symptoms of uterine cancer or are diagnosed with conditions, consult our experts at Manipal Hospitals, Dhakuria, for timely, personalised care you can trust.
FAQ's
Uterine cancers can be cured if they are detected early. Early detection allows for surgical removal of the uterus along with draining lymph nodes which is sufficient in the majority of cases to eliminate uterine cancer.
Abnormal vaginal bleeding is the most common sign—such as heavy periods, bleeding between cycles, or post-menopausal spotting. Other symptoms may include weight loss and bowel changes.
Women with a family history of uterine cancer or inherited conditions like Lynch syndrome are at higher risk. Other factors include obesity, Tamoxifen use, and unopposed oestrogen therapy.
Maintaining a healthy weight, using progestin/copper-releasing IUDs, taking combined (oestrogen + progestin) birth control pills, getting pregnant early, and having regular health checkups can help reduce uterine cancer risk.
You can schedule an appointment with a gynaecological oncologist at Manipal Hospitals, Dhakuria, by contacting us or visiting our website.
Visit: https://www.manipalhospitals.com/dhakuria/specialities/gynaec-oncology/
Contact no: 033 6907 0001






















 9 Min Read
9 Min Read